Medical Dermatology
Actinic Keratosis
- Home
- Medical Dermatology
- Skin Cancer
- Actinic Keratosis
Get Treatment for a Common Precancerous Skin Condition in the Dallas Area
 Do you have a spot or growth on your skin that you are unsure about? It may be an actinic keratosis. The Dallas area’s Dr. Ellen Turner can provide a thorough skin exam to look for this common sun-related lesion. By accurately diagnosing and treating an actinic keratosis, you can lower your risk of developing a more serious condition, have the lesion removed and replaced with healthy skin, and get relief for uncomfortable symptoms such as pain and tenderness.
Do you have a spot or growth on your skin that you are unsure about? It may be an actinic keratosis. The Dallas area’s Dr. Ellen Turner can provide a thorough skin exam to look for this common sun-related lesion. By accurately diagnosing and treating an actinic keratosis, you can lower your risk of developing a more serious condition, have the lesion removed and replaced with healthy skin, and get relief for uncomfortable symptoms such as pain and tenderness.
These lesions are called “precancerous” because they can sometimes develop into skin cancer if left untreated. This is why it’s important to get early diagnosis and treatment.
Medical Dermatology
Want to get diagnosis and care for actinic keratosis in the Dallas area? Submit a contact form to request an appointment or call (214) 903-4471.
What Is an Actinic Keratosis?
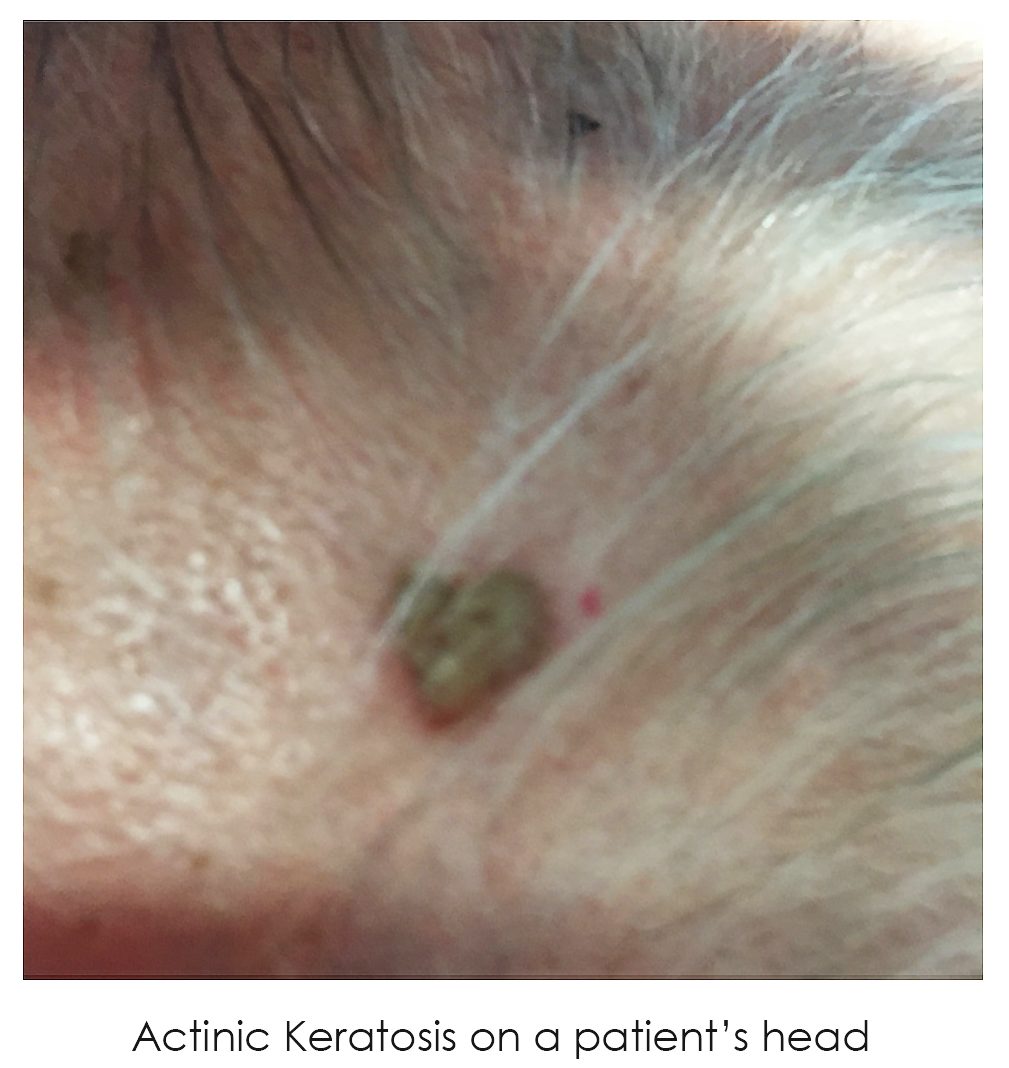
An actinic keratosis is a rough, scaly patch on the top layer of the skin. Sometimes an actinic keratosis might eventually harden and get a wartlike appearance. Common areas where an actinic keratosis can appear include the scalp, face, ears, neck, upper chest, arms, and the top of the hands. These are all areas that receive the most sun exposure, and the lesions develop due to years of cumulative UV damage. In most cases, an actinic keratosis is linked to frequent or intense exposure to ultraviolet rays from natural or artificial sources. It’s the most common type of precancerous skin condition.
“What are the red flags for actinic keratosis?” and “How do you tell the difference between actinic keratosis and skin cancer?” are some of the most common questions we get asked.
Although these lesions vary in appearance, some of the most typical symptoms are a patch of skin less than one inch in diameter with a rough, dry, or scaly texture; a flat or slightly raised bump that appears on the skin’s surface; and variations in color such as pink, red, or brown. You may experience itching, burning, bleeding, or crusting on the spot. It’s common for individuals to have multiple actinic keratosis lesions—known as “actinic keratoses” in plural. As the condition is often mistaken for a rash, it’s important to know what you’re looking for when you’re checking for signs of skin cancer.
What Are the Risk Factors for Actinic Keratosis?
Who is most at risk for developing an actinic keratosis? If you have a history of sun exposure over time, dating back as early as your childhood, you are at higher risk for actinic keratoses due to an accumulation of sun damage. Generally, individuals who don’t protect their skin from sun damage have the highest risk for this condition. You may also be at a higher risk of getting this condition if you have pale or fair skin, red or blond hair, or blue, green, or gray eyes. Other risk factors include the tendency to freckle or burn easily when exposed to sunlight, living in a very sunny area, being an older adult, having a history of multiple or severe sunburns, or having a weakened immune system.
How Is Actinic Keratosis Diagnosed?
By routine skin exam screening, a pre-cancer, also known as an actinic keratosis, can be fairly easy for a trained dermatologist to diagnose and treat. Often times, patients report “patches of dry or scaly skin” when the reality can be discreet scaly growths that are the result of an accumulation of UV exposure over many years, even in patients who currently do not get any sun exposure at all.
Patients can schedule an appointment with dermatologist Dr. Ellen Turner for a routine preventive skin body check to look for pre-cancers like actinic keratosis at her Dallas-area practice. These full body skin examinations for actinic keratosis also include checks for skin cancer and should be performed routinely once per year for patients who do not have a history of skin cancer or pre-cancer, and every six months for patients with a known history of the disease.
Check with a dermatologist such as Dr. Turner in order to determine whether you may have an actinic keratosis or pre-cancerous lesions.
What Is My Risk for Developing Skin Cancer if I Have an Actinic Keratosis?
Patients sometimes ask, “Should I worry about actinic keratosis?” Actinic keratosis is a precursor of the squamous cell cancer variant of nonmelanoma skin cancer. Typically, if left untreated, approximately 25 percent of these lesions can develop into squamous cell cancer. By addressing an actinic keratosis early, it can be cleared using a variety of treatments, thus preventing actual skin cancer from developing.
Which Procedures Are used to Treat an Actinic Keratosis?
If you have an actinic keratosis and get it treated at the early stage, it’s often possible to completely clear the lesion. So what gets rid of an actinic keratosis? Cases of precancerous lesions are expected to continue to rise for 2024, but potential treatment options have also increased. The most appropriate treatment option for you will depend on how many precancerous lesions you have, what they look like, your skin type, and the time of year.
Cryotherapy
Many times, liquid nitrogen can be used to pinpoint these lesions and cause destruction of the abnormal cells. When the treatment is performed properly by a trained dermatologist, scarring can be minimized or avoided. This procedure utilizing liquid nitrogen for its non-scarring destruction is called cryotherapy.
There are additional destructive treatments that can be used similarly, but to treat a higher number of lesions, in sun-damaged areas. Chemical peels work right away, and cause a “frosting” or white appearance to the skin when applied. After the first one or two days of application, the skin in the treated area begins to scale and peel, leaving behind new, undamaged skin cells.
Photodynamic Therapy
Another topical modality used for the treatment of broader areas of actinic keratosis and damage is photodynamic therapy (PDT). Photodynamic therapy involves the use of a chemical called aminolevulenic acid (ALA), which is applied to the surface to be treated. This chemical requires incubation of at least one hour, followed by activation by a particular light source: either a blue light or broadband or pulsed light. When activated by light, ALA causes a mild tingling in the treatment site. The activation allows treatment of sun-damaged skin cells by targeting and destroying those with abnormal DNA, forcing new cellular turnover. A period of redness, swelling, and resulting scaling and peeling typically occur over one to three weeks after a PDT treatment, depending on the location of the treatment—such as the face versus the arms.
Topical Creams
Additionally, there are topical creams that can be applied to the sun-damaged areas. The initial topical, which is still used in practice today, is a chemotherapy agent known as 5-fluorouracil (5-FU). This chemical induces a reaction that causes redness and resultant scaling and peeling to occur over one to three weeks of use. Once the treated area is inflamed and crusting, the treatment may be stopped and the area allowed to heal back to normal. There are also newer topical creams classified as immunomodulators. Imiquimod is a good example of an immunomodulatory treatment that can be used to address both pre-cancer and actinic keratoses, as well as some superficial skin cancers, such as basal cell carcinoma. There are many variations as to how imiquimod can be used for the treatment of an actinic keratosis, but it is typically applied to an area for two weeks, then stopped for two weeks, the re-initiated for two final weeks before completion at the end of a six-week period.
All treatments discussed in this section on actinic keratosis are non-scarring with variations as to the level of discomfort the patient will experience.
What Can You Do to Prevent an Actinic Keratosis?
Limiting sun exposure and taking steps to protect your skin against ultraviolet (UV) rays is often the best way to reduce your risk of developing an actinic keratosis. It is very important and necessary to wear sun protection and sunscreen daily! A time when most people receive exposure without necessarily realizing it is when they are driving in the car. Covering up with clothing and hats will help to provide extra protection for your skin. Avoid tanning beds, as they can be just as damaging as sun exposure.
What Else Is Available for Medical and Cosmetic Skin Care?
Along with diagnosis and care for many conditions that affect the skin—such as acne, actinic keratoses, skin cancer, rosacea, and psoriasis—Dr. Ellen Turner also offers a wide array of cosmetic skin care options. These include injectables such as neuromodulators like BOTOX® Cosmetic and dermal fillers, laser and light-based devices, and other skin rejuvenation or resurfacing options such as chemical peels and microneedling. Aesthetic procedures improve the look and feel of the skin.